- N
Meta-Analysis of 89 Structural MRI Studies in Posttraumatic Stress Disorder...
- neurovault.org
niftiUpdated Jul 20, 2018+ more versions Share
Share Facebook
Facebook Twitter
Twitter EmailClick to copy linkLink copied
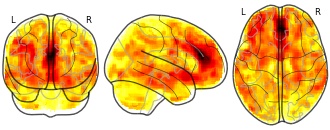
EmailClick to copy linkLink copied Cite(2018). Meta-Analysis of 89 Structural MRI Studies in Posttraumatic Stress Disorder and Comparison With Major Depressive Disorder: Meta-analysis result from 13 VBM studies: Hedges g effect size, gray matter volume (contrast is PTSDniftiAvailable download formatsUnique identifierhttps://identifiers.org/neurovault.image:65630Dataset updatedJul 20, 2018License
Cite(2018). Meta-Analysis of 89 Structural MRI Studies in Posttraumatic Stress Disorder and Comparison With Major Depressive Disorder: Meta-analysis result from 13 VBM studies: Hedges g effect size, gray matter volume (contrast is PTSDniftiAvailable download formatsUnique identifierhttps://identifiers.org/neurovault.image:65630Dataset updatedJul 20, 2018LicenseCC0 1.0 Universal Public Domain Dedicationhttps://creativecommons.org/publicdomain/zero/1.0/
License information was derived automaticallyDescriptionThe following inclusion criteria were applied to the database of 113 studies: 1) gray matter VBM study comparing adult patients with PTSD to either non-traumatised-controls or traumatised-controls; 2) results presented in Talairach or MNI coordinates; 3) studies were only included if a whole brain analysis was performed rather than a small volume correction to ensure no bias in the regions reported. Thirteen studies met inclusion criteria and are listed in Table S1. We emailed all study authors who used SPM (Statistical Parametric Mapping) to process their data for a ‘T-map’ image comparing PTSD gray matter volume to the control group. ‘T-maps’ are three dimensional maps comprising statistical data of volume differences in thousands of voxels in the brain and provide far more detailed information than significant coordinates reported in studies. However, SDM allows both T-maps and coordinates to be combined in a single meta-analysis and the methodology reported in detail by Radua et al. We received 6 T-maps from 6 independent studies and these were included in the meta-analyses. In addition to the main meta-analysis comparing PTSD to all controls, three additional VBM analyses were conducted: 1) comparing the PTSD group with non-traumatised-controls only 2) comparing the PTSD group with traumatised-controls only, 3) comparing PTSD group with all controls and widening the criteria to include paediatric studies. T-maps and coordinates signifying gray matter volume changes from where we were unable to obtain T-maps were extracted from relevant studies and analysed using Seed-based d Mapping (SDM version 5.14, http://www.sdmproject.com). For studies where coordinate data was used, these were convolved with a Gaussian kernel (FWHM=20mm) in order to optimally compensate the sensitivity and specificity of the analysis. As is standard in SDM analyses, the number of randomizations were set to 100 and a threshold was set at p<0.005 as well as a cluster-level threshold of 10 voxels in order to increase sensitivity and correctly control false-positive rate.8 A jackknife sensitivity analysis was performed in order to assess the robustness of the results which was achieved by excluding one study in each of the analyses.
Collection description
OBJECTIVE:
The authors conducted a comprehensive meta-analysis of MRI region-of-interest and voxel-based morphometry (VBM) studies in posttraumatic stress disorder (PTSD). Because patients have high rates of comorbid depression, an additional objective was to compare the findings to a meta-analysis of MRI studies in depression.METHOD:
The MEDLINE database was searched for studies from 1985 through 2016. A total of 113 studies met inclusion criteria and were included in an online database. Of these, 66 were selected for the region-of-interest meta-analysis and 13 for the VBM meta-analysis. The region-of-interest meta-analysis was conducted and compared with a meta-analysis of major depressive disorder. Within the region-of-interest meta-analysis, three subanalyses were conducted that included control groups with and without trauma.RESULTS:
In the region-of-interest meta-analysis, patients with PTSD compared with all control subjects were found to have reduced brain volume, intracranial volume, and volumes of the hippocampus, insula, and anterior cingulate. PTSD patients compared with nontraumatized or traumatized control subjects showed similar changes. Traumatized compared with nontraumatized control subjects showed smaller volumes of the hippocampus bilaterally. For all regions, pooled effect sizes (Hedges' g) varied from -0.84 to 0.43, and number of studies from three to 41. The VBM meta-analysis revealed prominent volumetric reductions in the medial prefrontal cortex, including the anterior cingulate. Compared with region-of-interest data from patients with major depressive disorder, those with PTSD had reduced total brain volume, and both disorders were associated with reduced hippocampal volume.CONCLUSIONS:
The meta-analyses revealed structural brain abnormalities associated with PTSD and trauma and suggest that global brain volume reductions distinguish PTSD from major depression.Subject species
homo sapiens
Modality
Structural MRI
Analysis level
meta-analysis
Cognitive paradigm (task)
2nd-order rule acquisition
Map type
Other
- f
Description of subgroups for analysis.
- plos.figshare.com
xlsUpdated Jun 6, 2025 Share
Share Facebook
Facebook Twitter
Twitter EmailClick to copy linkLink copied
EmailClick to copy linkLink copied CiteIwo Fober; Lidia Baran; Myrto Samara; Spyridon Siafis; David Robert Grimes; Bartosz Helfer (2025). Description of subgroups for analysis. [Dataset]. http://doi.org/10.1371/journal.pone.0325384.t004xlsAvailable download formatsUnique identifierhttps://doi.org/10.1371/journal.pone.0325384.t004Dataset updatedJun 6, 2025Dataset provided byPLOS ONEAuthorsIwo Fober; Lidia Baran; Myrto Samara; Spyridon Siafis; David Robert Grimes; Bartosz HelferLicense
CiteIwo Fober; Lidia Baran; Myrto Samara; Spyridon Siafis; David Robert Grimes; Bartosz Helfer (2025). Description of subgroups for analysis. [Dataset]. http://doi.org/10.1371/journal.pone.0325384.t004xlsAvailable download formatsUnique identifierhttps://doi.org/10.1371/journal.pone.0325384.t004Dataset updatedJun 6, 2025Dataset provided byPLOS ONEAuthorsIwo Fober; Lidia Baran; Myrto Samara; Spyridon Siafis; David Robert Grimes; Bartosz HelferLicenseAttribution 4.0 (CC BY 4.0)https://creativecommons.org/licenses/by/4.0/
License information was derived automaticallyDescriptionBackgroundDepression is a common mental disorder significantly impacting daily functioning. Standard treatments include drugs, psychotherapies, or a combination of both. Treatment selection relies on scientific evidence, though the trustworthiness and applicability of this evidence can vary.ObjectivesThis protocol presents a method to evaluate evidence from systematic reviews for pharmacological and psychological treatments for depression, focusing on trustworthiness and applicability structured into five components: quality of conduct and reporting, risk of bias, spin in abstract conclusions, robustness of meta-analytical results, heterogeneity and clinical diversity.MethodsWe will conduct a systematic search of systematic reviews in MEDLINE, Embase, PsycInfo, and Cochrane Database of Systematic Reviews. Our focus will be on systematic reviews of first-line treatments for depression in adults, including antidepressants, psychotherapy, or combined treatments, compared to either active or inactive comparators. We will extract information needed for a comprehensive methodological evaluation using qualitative tools, including AMSTAR 2, ROBIS, Conflict-of-Interest assessment, Referencing Framework for SRs, Spin Measure, and heterogeneity exploration assessment. For quantitative analyses, such as Fragility Index, Ellipse of Insignificance, Region of Attainable Redaction, GRIM test, Leave-N-Out analysis, and prediction intervals, we will select and recalculate two meta-analyses per review. We define a set of outcomes to enable practical and intuitive interpretation of these analyses’ results. Descriptive statistics, non-parametric statistical tests, and narrative summaries will be used to synthesize and compare outcomes across several pre-specified subgroups.Expected outcomesWe expect these analyses to provide an enhanced perspective on the practice of evidence synthesis in the field of mental health, offer methodological guidance for future systematic reviews and meta-analyses, and contribute to improved informed decision-making by clinicians and patients.OSF registrationosf.io/7f9cj and osf.io/ynejs
- f
Summary of eligibility criteria.
- plos.figshare.com
xlsUpdated Jun 6, 2025 Share
Share Facebook
Facebook Twitter
Twitter EmailClick to copy linkLink copied
EmailClick to copy linkLink copied CiteIwo Fober; Lidia Baran; Myrto Samara; Spyridon Siafis; David Robert Grimes; Bartosz Helfer (2025). Summary of eligibility criteria. [Dataset]. http://doi.org/10.1371/journal.pone.0325384.t001xlsAvailable download formatsUnique identifierhttps://doi.org/10.1371/journal.pone.0325384.t001Dataset updatedJun 6, 2025Dataset provided byPLOS ONEAuthorsIwo Fober; Lidia Baran; Myrto Samara; Spyridon Siafis; David Robert Grimes; Bartosz HelferLicense
CiteIwo Fober; Lidia Baran; Myrto Samara; Spyridon Siafis; David Robert Grimes; Bartosz Helfer (2025). Summary of eligibility criteria. [Dataset]. http://doi.org/10.1371/journal.pone.0325384.t001xlsAvailable download formatsUnique identifierhttps://doi.org/10.1371/journal.pone.0325384.t001Dataset updatedJun 6, 2025Dataset provided byPLOS ONEAuthorsIwo Fober; Lidia Baran; Myrto Samara; Spyridon Siafis; David Robert Grimes; Bartosz HelferLicenseAttribution 4.0 (CC BY 4.0)https://creativecommons.org/licenses/by/4.0/
License information was derived automaticallyDescriptionBackgroundDepression is a common mental disorder significantly impacting daily functioning. Standard treatments include drugs, psychotherapies, or a combination of both. Treatment selection relies on scientific evidence, though the trustworthiness and applicability of this evidence can vary.ObjectivesThis protocol presents a method to evaluate evidence from systematic reviews for pharmacological and psychological treatments for depression, focusing on trustworthiness and applicability structured into five components: quality of conduct and reporting, risk of bias, spin in abstract conclusions, robustness of meta-analytical results, heterogeneity and clinical diversity.MethodsWe will conduct a systematic search of systematic reviews in MEDLINE, Embase, PsycInfo, and Cochrane Database of Systematic Reviews. Our focus will be on systematic reviews of first-line treatments for depression in adults, including antidepressants, psychotherapy, or combined treatments, compared to either active or inactive comparators. We will extract information needed for a comprehensive methodological evaluation using qualitative tools, including AMSTAR 2, ROBIS, Conflict-of-Interest assessment, Referencing Framework for SRs, Spin Measure, and heterogeneity exploration assessment. For quantitative analyses, such as Fragility Index, Ellipse of Insignificance, Region of Attainable Redaction, GRIM test, Leave-N-Out analysis, and prediction intervals, we will select and recalculate two meta-analyses per review. We define a set of outcomes to enable practical and intuitive interpretation of these analyses’ results. Descriptive statistics, non-parametric statistical tests, and narrative summaries will be used to synthesize and compare outcomes across several pre-specified subgroups.Expected outcomesWe expect these analyses to provide an enhanced perspective on the practice of evidence synthesis in the field of mental health, offer methodological guidance for future systematic reviews and meta-analyses, and contribute to improved informed decision-making by clinicians and patients.OSF registrationosf.io/7f9cj and osf.io/ynejs
- f
Table 1_Craftwell: a feasibility and acceptability study of outdoor heritage...
- figshare.com
- frontiersin.figshare.com
docxUpdated Mar 5, 2025 Share
Share Facebook
Facebook Twitter
Twitter EmailClick to copy linkLink copied
EmailClick to copy linkLink copied CiteEmily Shoesmith; Patricia M. Darcy; Stephanie Piper; Piran C. L. White; Andy Needham; Aimée Little; Gareth Perry; Peter Coventry (2025). Table 1_Craftwell: a feasibility and acceptability study of outdoor heritage crafting for wellbeing and mental health.docx [Dataset]. http://doi.org/10.3389/fpubh.2025.1556230.s001docxAvailable download formatsUnique identifierhttps://doi.org/10.3389/fpubh.2025.1556230.s001Dataset updatedMar 5, 2025Dataset provided byFrontiersAuthorsEmily Shoesmith; Patricia M. Darcy; Stephanie Piper; Piran C. L. White; Andy Needham; Aimée Little; Gareth Perry; Peter CoventryLicense
CiteEmily Shoesmith; Patricia M. Darcy; Stephanie Piper; Piran C. L. White; Andy Needham; Aimée Little; Gareth Perry; Peter Coventry (2025). Table 1_Craftwell: a feasibility and acceptability study of outdoor heritage crafting for wellbeing and mental health.docx [Dataset]. http://doi.org/10.3389/fpubh.2025.1556230.s001docxAvailable download formatsUnique identifierhttps://doi.org/10.3389/fpubh.2025.1556230.s001Dataset updatedMar 5, 2025Dataset provided byFrontiersAuthorsEmily Shoesmith; Patricia M. Darcy; Stephanie Piper; Piran C. L. White; Andy Needham; Aimée Little; Gareth Perry; Peter CoventryLicenseAttribution 4.0 (CC BY 4.0)https://creativecommons.org/licenses/by/4.0/
License information was derived automaticallyDescriptionBackgroundThere has been increasing interest in creativity, heritage and nature to improve health-related outcomes. However, limited research has examined the intersection of heritage crafting in the context of natural spaces. This study aims to explore the feasibility and acceptability of an archaeologically informed outdoor heritage crafting intervention.MethodsA mixed-methods single group before and after feasibility study was conducted. Participants completed questionnaires, including validated items measuring outcomes related to mental health, wellbeing, social connectedness, mindfulness, perceived state of flow and the connection with nature and the environment. Qualitative interviews were conducted with participants to explore their experiences, and data were analyzed using thematic analysis.ResultsForty-eight participants from a University in the United Kingdom attended the workshops, achieving the recruitment target within the required timeframe. The response rate to all pre-workshop measures was 100% and remained at 100% post-workshop, with the exception of missing data for two participants (4.2%) for measures assessing wellbeing and anxiety, and missing data for five participants (10.4%) for the measure assessing depression. Therefore, response and retention rates indicate high levels of feasibility to conduct a robust evaluation of this intervention. Five themes were identified, including: participant motivation to sign up; engaging with creative activities in a natural setting; skilled facilitation and a flexible approach; group delivery, and duration and frequency of workshops. Overall, the workshops were positively received by participants, primarily attributing their satisfaction to engagement with group-based creative activities in a natural setting with an educational component.ConclusionThis study has shown it is feasible and acceptable to deliver and evaluate an archaeologically informed heritage crafting intervention to support wellbeing. These results suggest the need for formal testing of the potential health benefits of the intervention to address policy imperatives for developing and implementing community- and place-based approaches to support mental health.
Not seeing a result you expected?
Learn how you can add new datasets to our index.
 Facebook
Facebook Twitter
TwitterMeta-Analysis of 89 Structural MRI Studies in Posttraumatic Stress Disorder and Comparison With Major Depressive Disorder: Meta-analysis result from 13 VBM studies: Hedges g effect size, gray matter volume (contrast is PTSD
CC0 1.0 Universal Public Domain Dedicationhttps://creativecommons.org/publicdomain/zero/1.0/
License information was derived automatically
The following inclusion criteria were applied to the database of 113 studies: 1) gray matter VBM study comparing adult patients with PTSD to either non-traumatised-controls or traumatised-controls; 2) results presented in Talairach or MNI coordinates; 3) studies were only included if a whole brain analysis was performed rather than a small volume correction to ensure no bias in the regions reported. Thirteen studies met inclusion criteria and are listed in Table S1. We emailed all study authors who used SPM (Statistical Parametric Mapping) to process their data for a ‘T-map’ image comparing PTSD gray matter volume to the control group. ‘T-maps’ are three dimensional maps comprising statistical data of volume differences in thousands of voxels in the brain and provide far more detailed information than significant coordinates reported in studies. However, SDM allows both T-maps and coordinates to be combined in a single meta-analysis and the methodology reported in detail by Radua et al. We received 6 T-maps from 6 independent studies and these were included in the meta-analyses. In addition to the main meta-analysis comparing PTSD to all controls, three additional VBM analyses were conducted: 1) comparing the PTSD group with non-traumatised-controls only 2) comparing the PTSD group with traumatised-controls only, 3) comparing PTSD group with all controls and widening the criteria to include paediatric studies. T-maps and coordinates signifying gray matter volume changes from where we were unable to obtain T-maps were extracted from relevant studies and analysed using Seed-based d Mapping (SDM version 5.14, http://www.sdmproject.com). For studies where coordinate data was used, these were convolved with a Gaussian kernel (FWHM=20mm) in order to optimally compensate the sensitivity and specificity of the analysis. As is standard in SDM analyses, the number of randomizations were set to 100 and a threshold was set at p<0.005 as well as a cluster-level threshold of 10 voxels in order to increase sensitivity and correctly control false-positive rate.8 A jackknife sensitivity analysis was performed in order to assess the robustness of the results which was achieved by excluding one study in each of the analyses.
Collection description
OBJECTIVE:
The authors conducted a comprehensive meta-analysis of MRI region-of-interest and voxel-based morphometry (VBM) studies in posttraumatic stress disorder (PTSD). Because patients have high rates of comorbid depression, an additional objective was to compare the findings to a meta-analysis of MRI studies in depression.
METHOD:
The MEDLINE database was searched for studies from 1985 through 2016. A total of 113 studies met inclusion criteria and were included in an online database. Of these, 66 were selected for the region-of-interest meta-analysis and 13 for the VBM meta-analysis. The region-of-interest meta-analysis was conducted and compared with a meta-analysis of major depressive disorder. Within the region-of-interest meta-analysis, three subanalyses were conducted that included control groups with and without trauma.
RESULTS:
In the region-of-interest meta-analysis, patients with PTSD compared with all control subjects were found to have reduced brain volume, intracranial volume, and volumes of the hippocampus, insula, and anterior cingulate. PTSD patients compared with nontraumatized or traumatized control subjects showed similar changes. Traumatized compared with nontraumatized control subjects showed smaller volumes of the hippocampus bilaterally. For all regions, pooled effect sizes (Hedges' g) varied from -0.84 to 0.43, and number of studies from three to 41. The VBM meta-analysis revealed prominent volumetric reductions in the medial prefrontal cortex, including the anterior cingulate. Compared with region-of-interest data from patients with major depressive disorder, those with PTSD had reduced total brain volume, and both disorders were associated with reduced hippocampal volume.
CONCLUSIONS:
The meta-analyses revealed structural brain abnormalities associated with PTSD and trauma and suggest that global brain volume reductions distinguish PTSD from major depression.
Subject species
homo sapiens
Modality
Structural MRI
Analysis level
meta-analysis
Cognitive paradigm (task)
2nd-order rule acquisition
Map type
Other